
KEMRI Hosts Ugandan Team for Knowledge and Grants Management Exchange
November 12, 2025
AMR: Harbinger of Global Health Disaster
November 19, 2025KEMRI’s Warns of Escalating AMR Crisis in the Country
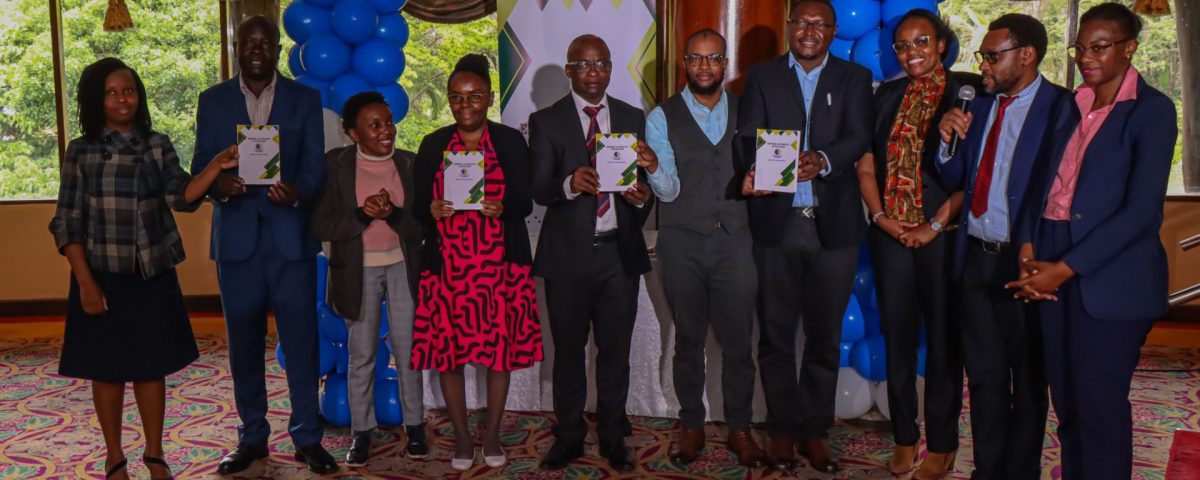
The Institute has sounded an urgent alarm over rising antimicrobial resistance (AMR) following new research showing a sharp increase in multidrug-resistant infections across Nairobi. The findings, released by the Centre for Microbiology Research (CMR), coincided with a recent national launch of the Antimicrobial Guidelines last week on Wednesday, 12th November 2025 at a Nairobi Hotel.
According to CMR, fresh surveillance data from Mama Lucy Kibaki Hospital (MLKH) in Nairobi County shows that over 45 percent of typhoid fever cases are now linked to multidrug-resistant Salmonella Typhi. Equally concerning are insights from investigations into the 2022 cholera outbreak, where Vibrio cholerae O1 (Ogawa serotype) was confirmed as the causative strain with 99 percent of which showed multidrug resistance.
These revelations come as Kenya joins the world in marking the 2025 Global Antimicrobial Awareness Week, underscoring the urgency of intensified stewardship and evidence-based clinical practice.
At the Nairobi launch, KEMRI scientists Dr. Cecilia Mbae, Dr. Peter Muturi, and Dr. Susan Kavai emphasized the critical role of research and surveillance in containing the AMR threat not just in Nairobi County, but throughout the country and region. Dr. Mbae, also the Ag. Deputy Director in charge of CMR, highlighted the gravity of the situation, noting that KEMRI’s public health mission has never been more relevant.
“At KEMRI, our mission is deeply rooted in public health: to improve the quality of human health through research, innovation, capacity development and service delivery. This mission has guided our work for decades, and nowhere is it more relevant than in our collective fight against AMR, a silent but escalating global health threat,” she said.


For more than a decade, CMR has led national monitoring of resistance patterns in key enteric pathogens, including Salmonella, Shigella, Vibrio cholerae and diarrhoeagenic E. coli, particularly in Nairobi’s informal settlements and other high-risk regions. These organisms remain among the leading causes of diarrhoeal diseases affecting children and immunocompromised populations.
According to Dr. Mbae, recent CMR data now confirms a steady rise in multidrug resistance, including increasing reduced susceptibility to fluoroquinolones. Since 2021, KEMRI has partnered with MLKH on continuous pathogen surveillance to guide clinical decisions and influence national health policy.
She described the new antimicrobial guidelines as “a pivotal step” in translating science into action thus, “these guidelines represent a critical step forward in transforming research and surveillance data into practical clinical action. Let us commit to using antibiotics only when necessary and when evidence supports their use. Let us strengthen laboratory guided therapy and continue AMR surveillance to track emerging patterns.”
She reaffirmed KEMRI’s commitment to supporting the initiative through ongoing surveillance, data sharing, and enhanced laboratory capacity.
During a panel session, Dr. Muturi warned that AMR, projected to cause up to 10 million deaths annually by 2050, remains a preventable global catastrophe if countries act urgently.
He underscored the need for strong hospital–research partnerships, continuous training of healthcare workers, mentorship programmes, and robust community health engagement to drive prudent antimicrobial use and improve clinical outcomes.
He stressed the importance of strong hospital research institution partnerships to advance antimicrobial stewardship, improve surveillance, and promote evidence-based prescribing.
With AMR rising at an alarming pace, last week’s AMR Guideline launch and AMR Awareness Week sets the stage for strengthened coordination, enhanced preparedness, and renewed national commitment to safeguarding the efficacy of life-saving medicines.

