2nd Health & Climate Change Conference,
28th & 30th August 2023
HEALTH AND CLIMATE CHANGE CONFERENCE
Theme: “Towards Delivery of Climate Resilient Universal Health Coverage (UHC) Leveraging on Blue and Green Economy”
Date: 28th to 30th August, 2023
Venue: Diamond Leisure Beach and Golf Resort Diani, Kwale County
Background and Rationale
1.1 Background
COVID-19 pandemic is the greatest global crisis in decades. Over 6.6 million of Hundreds of lives have been lost and has triggered the largest world economic crisis. This has resulted to loss of employment and income as a result of the lockdowns which has caused further damage to livelihoods, health, and sustainable development (WHO, 2020). In addition, as a result of these gaps, communities need to protect themselves for quick recovery from the pandemic. However, we may not go back to the way we did things before from the lessons learnt. Increasing numbers of emerging and re-emerging infectious diseases, including HIV/AIDS, SARS and Ebola, from exposure from exposure of humans to zoonotic pathogens and all available evidence suggests that COVID-19 may have followed the same route.
When COVID-19 transmission from human-to-human began, it spread very fast across boarders because national and international surveillance and rapid response systems were either not strong or fast enough to completely halt transmission. Lack of universal health coverage both in low- and medium-income countries, including many in rich countries has left billions of individuals without reliable and affordable access to medical treatment (WHO, 2020). Deaths and loss of livelihoods has been as a result of great inequalities strongly driven by socioeconomic status, which is often compounded by gender and minority status, despite the global commitment not to leave anybody behind in respect to access of health services. There is need to address environmental protection, emergency preparedness, health systems, and social safety nets by government allocating resources because when pandemics or disasters strike the bill will be many times over. There is urgent need to address these issues because the world cannot afford repeated catastrophes on the magnitude of COVID-19, whether caused by the next pandemic, or from increasing environmental degradation, air pollution and climate change.
Lessons learnt COVID-19 pandemic has shown that people will support even difficult policies if decision-making is transparent, evidence-based, and inclusive (WHO, 2020). These policies have clear goal of protecting their well-being with their families rather than serving special interests. Opinion polls from around the world show that people want to protect the environment and preserve the positives that have emerged from the pandemic, as we recover (WHO, 2020). Therefore, this needs to be reflected in the way that policy is made.
To recover from the effects of COVID-19, most finance ministries in most countries will come up with economic recovery packages and policy decisions. Given the fundamental connection between the environment, air pollution, health and the economy, it is also important that health leaders, such as health managers are directly involved in their design, report on the short and long-term public health impacts that they may have and give their endorsement of approval.
National governments are now pledging billions of dollars, to maintain and eventually revive economic activities. These investments are essential to safeguard people’s livelihoods, and subsequently their health. However, the allocation of these investments, and the policy decisions will guide both short- and long-term recovery and have the potential to shape the way we live our lives, work and consume for years to come. Nowhere is this more important than in their effects on environmental degradation and pollution, and particularly on the greenhouse gas emissions that are driving global warming and the climate crisis (WHO, 2020).
1.2 Rationale of The Conference
1.2.1. WHO Perspective Rationale
The WHO Prescriptions for a healthy, green recovery which forms the basis of this conference include but not limited to: –
1) Protect and preserve the source of human health: Nature
Economies are a product of healthy human societies, which in turn rely on the natural environment – the original source of all clean air, water, and food. Human pressures, from deforestation, to intensive and polluting agricultural practices, to unsafe management and consumption of wildlife, undermine these services. They also increase the risk of emerging infectious diseases in humans – over 60% of which originate from animals, mainly from wildlife. Overall plans for post-COVID-19 recovery, and specifically plans to reduce the risk of future epidemics, need to go further upstream than early detection and control of disease outbreaks. They also need to lessen our impact on the environment, to reduce the risk at source.
2) Invest in essential services, from water and sanitation to clean energy in healthcare facilities.
Around the world, billions of people lack access to the most basic services that are required to protect their health, whether from COVID-19, or any other risk. Handwashing facilities are essential for the prevention of infectious disease transmission but are lacking in 40 % of households. Antimicrobial-resistant pathogens are widespread in water and waste and their sound management is needed to prevent the spread back to humans.
It is essential that health care facilities be equipped with water and sanitation services, including the soap and water that constitutes the most basic intervention to cut transmission.
Overall, avoidable environmental and occupational risks cause about one quarter of all deaths in the world. Investment in healthier environments for health protection, environmental regulation, and ensuring that health systems are climate resilient, is both an essential guardrail against future disaster, and offers some of the best returns for society.
3) Ensure a quick healthy energy transition.
Currently, 85% of more than 900 million people rely on polluting fuels in Sub-Saharan Africa (SSA) which is the highest dependence globally. About 683,984 (8.9% of total mortality) people die yearly from exposure to household air pollution in the same region. Over 90% of people breathe outdoor air with pollution levels exceeding WHO air quality guideline values. Two-thirds of this exposure to outdoor pollution results from the burning of the same fossil fuels that are driving climate change. At the same time, renewable energy sources and storage continue to drop in price, increase in reliability, and provide more numerous, safer and higher paid jobs. Energy infrastructure decisions taken now will be locked in for decades to come.
Factoring in the full economic and social consequences, and taking decisions in the public health interest, will tend to favour renewable energy sources, leading to cleaner environments and healthier people.
4) Promote healthy, sustainable food systems.
Diseases caused by lack of access to food as a result of droughts, unhealthy diets. These unhealthy diets also increase vulnerability to other health conditions such as obesity and diabetes which are among the largest risk factors for illness and death from COVID-19.
A quarter of global greenhouse gases is as a result of Agriculture. This is particularly as a result of clearing of land to rear livestock and farming. This is the single biggest environmental driver of new disease outbreaks. Therefore, there is a need for a rapid transition to healthy, nutritious and sustainable diets as prescribed in the WHO’s dietary guidelines. This would save millions of lives, reduce disease risks, and bring major reductions in global greenhouse gas emissions.
5) Build healthy, liveable cities.
Over half of the world’s population now lives in cities. They are responsible for over 60% of both economic activity and greenhouse gas emissions. Cities have relatively high population densities and are traffic-saturated, many trips can be taken more efficiently by public transport, walking and cycling, than by private cars. This also brings major health benefits through reducing air pollution, road traffic injuries – and the over three million annual deaths from physical inactivity.
6) Stop using taxpayers’ money to fund pollution.
The economic damage from COVID-19 and the necessary control measures, is very real, and will place huge pressure on Government finances. Financial reform will be unavoidable in recovering from COVID-19, and a good place to start is with fossil fuel subsidies.
Placing a price on polluting fuels in line with the damage they cause would approximately halve outdoor air pollution deaths, cut greenhouse gas emissions by over a quarter, and raise about 4% of global GDP in revenue. We should stop paying the pollution bill, both through our pockets and our lungs.
The health community is increasingly an ally in this goal. Community Health Workers are the single most trusted profession in the world. Their skill, dedication, bravery and compassion has saved countless lives during the COVID-19 pandemic raising them to even higher levels of respect in their communities. Health professionals from around the world have shown that they are also strong supporters of action to protect the environment – and thereby the health of the populations that they serve. They are ready to be champions for the green, healthy and prosperous societies of the future.
1.2.2 Country Perspective Rationale
Consensus shows climate change is already damaging human health and healthcare delivery and will have a greater impact in the future. Kenya’s improvements in the control of malaria, water-borne diseases, respiratory diseases, infant mortality, and malnutrition are at risk from setbacks relating to climate change (https://www.kenyamarkets.org/wp-content/uploads/2019/02/NCCAP-2018-2022-Online-.pdf). The economic cost of the loss of productivity from pollution-related diseases are estimated to be up to 2.0% of gross domestic product (GDP) (https://www.undp.org/sites/g/files/zskgke326/files/migration/ke/Final-Draft-GreenMark-Standard-for-Green-Buildings—20180918.pdf). These and many other potential impacts require not only continued investment and focus on climate sensitive health issues, but also full integration of climate change into Kenya’s many existing health programmes and policies being driven through the universal healthcare delivery framework(https://www4.unfccc.int/sites/NAPC/Documents%20NAP/Kenya_NAP_Final.pdf).
The health sector has a substantial role to play in both mitigating climate change through the adoption of low-carbon strategies, while also building resilience to climate impact in ways that plan for environmental change and expanded health threats (https://documents1.worldbank.org/curated/en/322251495434571418/pdf/113572-WP-PUBLIC-FINAL-WBG-Climate-smart-Healthcare-002.pdf). Taken together, these efforts comprise a “climate-smart” approach that will help health planners and decision-makers adjust to a new era of climate reality while improving health, environment, and development (https://documents1.worldbank.org/curated/en/322251495434571418/pdf/113572-WP-PUBLIC-FINAL-WBG-Climate-smart-Healthcare-002.pdf).
The causes of climate change are multi-sectoral in nature and therefore require a broad range of actors. However, implementation of climate-smart healthcare interventions by different sectors is not well coordinated resulting in duplication of efforts. There is a strong case for harnessing synergy in the efforts of the climate change and health stakeholders to catalyse the impacts of activities implemented across the stakeholder sectors (https://scalingupnutrition.org/wp-content/uploads/2013/10/Kenya-National-Nutrition-Action-Plan-2012-2017-final.pdf).
In this regard, the Ministry of Health in conjunction with the Ministries of Environment and Energy is organizing the second Environment, Climate Change and Health Conference to discuss how climate-smart health systems can enhance the Delivery of Universal Health coverage. The Conference is aimed at educating the public and healthcare professionals about the health effects of Environment, Air Pollution, Climate Change, and how climate change policy and consumption choices influence the health of our communities.
It will provide an opportunity to disseminate climate and health tools and resources to help healthcare practitioners set goals and implement strategies to reduce their climate impacts, ensure continuity of care in extreme weather events, and protect community health and well-being.
2.0 Purpose
2.1 Conference objectives:
- Disseminate available guidelines, technical tools, indicators and best practices to help the Ministry of Health and Counties in planning, programming and implementation of climate-smart initiatives.
- Build evidence for advocacy on resource allocation and financing for climate-smart health systems both at National and County level.
- Provide a platform for networking among different stakeholders (policy, research, civil society and private sector) to leverage on existing and future opportunities for advancing the climate-smart healthcare delivery.
- Define the strategies that will facilitate mainstreaming and integration of Energy, Air pollution and climate change into the UHC planning, programming and implementation:
- Strengthen multi-sectoral coordination mechanisms and networks for climate-smart healthcare at all levels.
- Disseminate government of Kenya commitment and implementation on air pollution, health and climate change during COP27
2.2 Conference outcomes:
- Enhanced awareness of health and environment sector practitioners on the connections between climate change and human health.
- Formation of a collaborative network of key stakeholders / Formation of strategic partnerships for the delivery of climate-smart Universal healthcare in Kenya
- Documentation of lessons learnt and best practices on climate-smart health systems to inform wider planning and implementation across government agencies.
- Formulation of a prioritized national climate and health research agenda in order to support evidence-based policy and intervention formulation, identifying gaps and critical factors for climate-smart health care
- Coordinated plan of action for the National and County governments on development of climate-smart health systems for climate change mitigation.
3.0 Scope of the conference
This conference will provide a forum for the presentation and discussion of the following agenda:
3.1 Climate-friendly healthcare infrastructure and technologies:
Health infrastructure relates to all the physical infrastructure, non-medical equipment, transport, and technology infrastructure (including ICT) required for effective delivery of services by the national and county governments and other health service providers (http://publications.universalhealth2030.org/uploads/kenya_health_policy_2014_to_2030.pdf). Hospitals exist to treat patients. However, as an industry it achieves her objective by consuming vast quantities of energy, food and water. In return, this industry produces million tons of Healthcare Waste and high volumes of greenhouse gases annually. It is expected by using efficient and renewable energy sources, reducing the use of disposables, eliminating unnecessary chemicals and changing food-buying policies, hospitals can help build a more sustainable environment and cut costs.
The conference will prepare healthcare facilities to adopt best available low carbon technology and best environmental practice.
Topics to be covered will include planning and green hospital buildings and landscapes; access to sustainable energy services in health care facilities using modern (including renewable) and efficient energy technologies while reducing energy vulnerability; efficient use and management of water; sustainable management of healthcare wastes; as well as improved access to quality food and nutritional care in hospitals.
3.2 Health in Climate Emergencies:
Climate-induced disasters such as floods, landslides, drought, fires, and earthquakes affect “the provision of healthcare by increasing the spread of infectious disease, and by reducing the opportunities to access healthcare due to the destruction of health infrastructure and the effects of the disasters on people’s ability to reach health facilities.”
The conference will discuss and disseminate available ‘prescriptions’ (toolkits/strategies) for climate-resilient emergency healthcare delivery.
3.3 Evidence-based decision-making through research:
There is need for enhancing evidence-based decision-making through operations research for purposes of strengthening the foundation of informed climate-smart healthcare program development and service provision.
The Conference will collate and disseminate evidence of best practices, assessment of current situation and of the resources that can be mobilized to address the gaps, to inform policy, programme design and implementation.
- Dissemination of climate and health research findings
3.4 Coordination and partnerships among the key Air pollution, climate change and sustainable healthcare actors.
The government acknowledges that a “Health in All Policies” approach is crucial to the realization of health goals. This approach ensures that the health sector interacts with and influences the design, implementation, and monitoring of interventions in all of the sectors that have an impact on health (http://publications.universalhealth2030.org/uploads/kenya_health_policy_2014_to_2030.pdf). Climate Smart healthcare programmes therefore need to look beyond the health sector and must be addressed through integrated approach for successful achievement of its goal. It requires the involvement of a broad range of actors including Planning, Environment, Energy, Infrastructure, Housing, Agriculture, Industry and Trade.
This conference therefore provides an opportunity to strengthen multi-sectoral coordination mechanisms and networks for climate-smart healthcare at all levels.
3.5 Investing in Air pollution, Climate Change and Health
Reduced exposure to climate sensitive conditions and diseases through low-carbon and resilience strategies for the health Sector will be critical to sustain the affordable healthcare interventions. This will greatly reduce the burden and budget related to treatment, leading to increased economic investments through out-of-pocket savings derived from UHC and initiatives motivated by a healthy human resource.
4.0 Targeted Audience:
The conference will bring together a mix of policy makers (national and county), researchers, academics, private sector and development practitioners in public health, energy, environment, built environment). It is anticipated that a maximum of 500 delegates will attend the conference both from government and public institutions
Refences:
- World Health Organization. WHO Manifesto for a healthy recovery from COVID-19. Prescriptions fo a healthy and green recovery from COVID-19. Geneva: World Health Organization; 2020 (https://breathelife2030.org/news/manifesto-healthy-recovery-covid-19/)
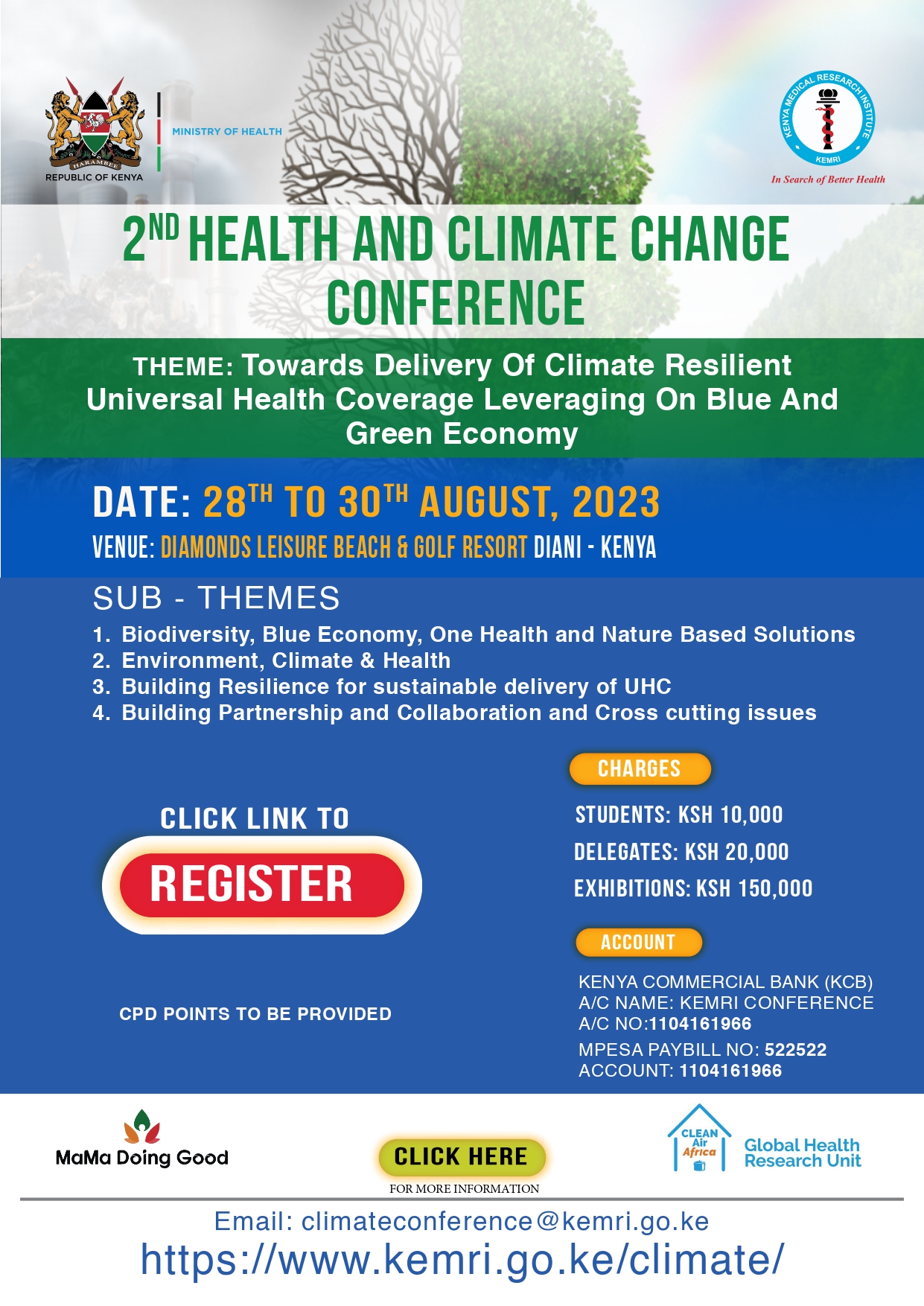
HEALTH AND CLIMATE CHANGE CONFERENCE THEMES
Main Theme;
Towards Delivery of Climate Resilient Universal Health Coverage Leveraging on Blue and Green Economy
Sub-themes;
- Biodiversity, Blue Economy, One health and nature-based solutions – the science and evidence
- Environment, climate & health – the science and evidence
- Building Resilience for sustainable delivery of UHC
- Building Partnership and collaboration and Cross cutting issues
Abstract Submission for the 2nd Health and Climate Change Conference
The organizing committee invites abstracts for papers and posters from any of the thematic areas to be presented in the conference. Submissions should be made by midnight 4th August 2023 to the scientific committee. All abstracts have to be submitted online. Abstracts submitted by post, fax or mail cannot be accepted.
General Guidelines and Rules for Abstract Submission apply. You will receive immediate confirmation of successful abstract submission. Please note that authors whose abstracts are accepted for presentation will be expected to attend the meeting and give their presentation.
All abstracts must be in English. The maximum word count is 300 words in Microsoft Word and the Font is Arial 11.5. This limit does not include the title. Your abstract should be structured in the format outlined below.
Abstract format
The abstract submitted should contain concise statements of:
Background: indicate the purpose and objective of the research, the hypothesis that was tested or a description of the problem being analyzed or evaluated.
Methods: describe the study period/setting/ location, study design, study population, data collection and methods of analysis used.
Results: present as clearly and in as much detail as possible the findings/outcome of the study. Please summarize any specific results.
Conclusions: explain the significance of your findings/outcomes of the study
To submit your abstract, CLICK HERE
PROGRAMME FOR THE 2ND HEALTH AND CLIMATE CHANGE CONFERENCE
COMING SOON
IMPORTANT DATES AND INFORMATION
Abstract Submission Deadline
4thAugust 2023
Conference Dates
28th -30th August 2023
REGISTRATION
2nd Health and Climate Change Conference Registration fee is payable to:
| Category | Charges |
| Student | 10,000 |
| Delegates | 20,000 |
| Exhibition Booth | 150,000 |
BANKING DETAILS;
NAME OF BANK: KENYA COMMERCIAL BANK(KCB)
ACCOUNT NAME: KEMRI CONFERENCE
ACCOUNT NUMBER: 1104161966
MPESA PAYBILL No: 522522
REGISTRATION FEE IS NON-REFUNDABLE
GET TO KNOW YOUR SPEAKERS

Dr. James Mwitari
Dr Mwitari is a long serving Public Health Practitioner with over 30 years’ experience in public health with substantial expertise in teaching, research, and leadership. He is currently working for KEMRI- Clean Air (Africa) Global Health Research unit as a Senior Research Fellow, Principal Investigator and Co-Director of the unit. He was formerly the Dean school of Public Health and Senior lecture in the Department of Health Systems at Amref international University. Dr Mwitari received his PhD in Epidemiology from Jomo Kenyatta University of Agriculture and Technology, Kenya, and holds an MSc in Communicable Disease Epidemiology (University of London, UK).
Dr. Mwitari has worked in various departments within the Kenyan Ministry of Health as well as the Ministry of Planning and National Development. His last title in the ministry of health was Deputy Director of Public Health. He now leads several international research projects on air pollution, energy and global public health including UK NIHR and FCDO funded research on technical solutions to clean energy access in informal settlements of Nairobi.
Prof. Sam Kariuki
Sam Kariuki (DVM, MSc, PhD) obtained his DVM from the University of Nairobi (1989), MSc in Pharmacology and Toxicology, University of Nairobi (1991), and a PhD in Tropical Medicine from the Liverpool School of Tropical Medicine (LSTM) in 1997. He was awarded Doctor of Science (Honoris causa) by the LSTM in December 2022. Currently he is Director, Drugs for Neglected Diseases Initiative (DNDi) East Africa Regional Office. Previously, he was Acting Director General at the Kenya Medical Research Institute (KEMRI) (2021-2023) and Director of Research and Development (2018-2022). He is Fellow, African Academy of Sciences and a Honorary Faculty Wellcome Sanger Institute, visiting Professor of Tropical Microbiology, Nuffield Department of Medicine, University of Oxford, and the Ohio State University One-Health Initiative. He is also a member of the American Society for Microbiology and Section Editor, Journal of Medical Microbiology.
Over the last 20 years his team has researched and published on epidemiology and genomics of Antimicrobial Resistance (AMR) and genomic surveillance of key enteric pathogens endemic in Kenya and the region, including typhoid fever, invasive non-typhoidal salmonella, cholera and E. coli infections. He has published over 200 papers in peer-reviewed journals and written 4 chapters in textbooks of Microbiology and Infectious Diseases, majoring in Genomics and Epidemiology. For his early work on the anthroponotic transmission of Salmonella Typhimurium invasive bloodstream infections in children less than 5 years of age and resulting in extremely high mortality rates in Kenya and the region (Kariuki et al. J Med Microbiol. 2006; 55(Pt 5):585-91), he won the prestigious Pfizer Prize (The Royal Society) for African Scientist of the Year Award, 2012.
As an expert in Antimicrobial Resistance surveillance and monitoring, he was selected as a member of the National Antimicrobial Stewardship Interagency Committee (NASIC) advising Ministry of Health on One Health approach in implementation of the National Action Plan to combat AMR. As a World Health Organization consultant for the last 15 years (WHO-AGISAR), he has provided technical advice and opinion in areas of food safety, antimicrobial resistance and infectious disease surveillance for Kenya and the region, and this has been through participating in various committees. In 2020, he was appointed as a member of the WHO Strategic and Technical Advisory Group for Antimicrobial Resistance (STAG-AMR).


Venue
Diamonds Leisure Beach and Golf Resort, Diani, Kwale County.
About Kenya- https://magicalkenya.com/








